Cervical Cancer Screening: Pap and HPV Tests

Each year, more than 13,000 women are diagnosed with cervical cancer in the United States. Yet cervical cancer is one of the most preventable cancers today. In most cases cervical cancer can be prevented through early detection and treatment of abnormal cell changes that occur in the cervix years before cervical cancer develops.
We now know that these cell changes are caused by human papillomavirus, commonly known as HPV. The traditional test for early detection has been the Pap test. For women age 30 and over, an HPV test is also recommended. HPV tests can find any of the high-risk types of HPV that are commonly found in cervical cancer.
Current guidelines for cervical cancer screening are:
- Women should start screening with the Pap test at age 21. (Screening is not recommended for women under age 21.)
Starting at age 30, women have three options available for screening:
- A Pap test alone every three years
- Co-testing with a Pap and HPV test, every five years
- An HPV test alone, every five years
Depending on the results of the Pap and/or HPV tests, a healthcare provider may recommend additional screening or procedures, so some women may be screened more often.
Don’t worry about which option is the best one for you: the exact test or tests used is not as important as simply being screened regularly! Your healthcare provider will help you sort out which option is right for you.
After age 65, women older than 65 who have had adequate prior screening and are not otherwise at high risk can stop screening. Women who have had a hysterectomy (with removal of the cervix) also do not need to be screened, unless they have a have a history of a high-grade precancerous lesions.
Pap Tests
 The Pap test finds changes in the cells of the cervix (the mouth of the womb) that are not normal. During a Pap test, the patient is positioned on an exam table and a device called a speculum (pictured to the right) is gently inserted to open the vagina. The speculum allows the health care provider to view the cervix and upper vagina.
The Pap test finds changes in the cells of the cervix (the mouth of the womb) that are not normal. During a Pap test, the patient is positioned on an exam table and a device called a speculum (pictured to the right) is gently inserted to open the vagina. The speculum allows the health care provider to view the cervix and upper vagina.
Once the provider can see the cervix, a brush will be used to collect some cells. The cells are sent to a laboratory where they are prepared and evaluated under a microscope.
The Pap test looks for any abnormal or precancerous changes in the cells on the cervix. If the Pap test results show these cell changes, this is usually called cervical dysplasia. Other common terms the healthcare provider may use include:
- Abnormal cell changes
- Precancerous cells changes
- CIN (cervical intraepithelial neoplasia)
- SIL (squamous intraepithelial lesions)
- “Warts” on the cervix
All of these terms mean similar things—it simply means that abnormalities were found. Most of the time, these cell changes are due to HPV. There are many types of HPV that can cause cervical dysplasia. Most of these types are considered “high-risk” types, which means that they have been linked with cervical cancer.
Just because a woman has cervical dysplasia, it does not mean she will get cervical cancer. It means that her healthcare provider will want to closely monitor her cervix every so often—and possibly do treatment—to prevent further cell changes that could become cancerous over time if left unchecked.
HPV Tests
HPV tests can find any of the high-risk types of HPV that are most commonly found in cervical cancer. The presence of any of these HPV types for many years can lead to cell changes that may need to be treated so that cervical cancer does not occur. An HPV test can be done alone, or with co-testing the HPV test is done at the same time as the Pap test.
Two high-risk HPV types, HPV 16 and HPV 18, are responsible for about 70% of cervical cancers worldwide. Knowing if a woman has these types of HPV gives healthcare providers more insight into her risk for developing cervical cancer.
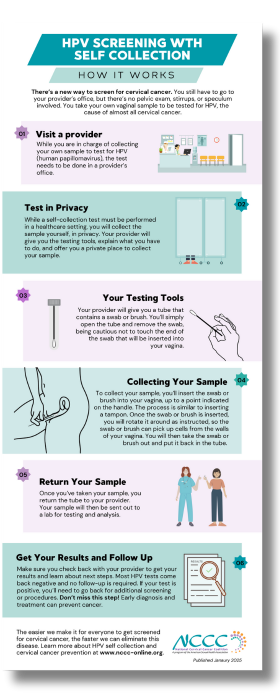
HPV Testing with Self Collection
If you’re doing an HPV test alone, you may be able to avoid the pelvic exam and speculum. The FDA recently approved tests that allow you to collect your own specimen from your vagina. That specimen will then be sent to a lab to check for the presence of HPV, and specifically for the high-risk types of the virus that cause cervical cancer.
This test can’t be done at home. You still have to go to a provider’s office, but you do not need a pelvic exam. Instead, your provider will give you a kit that includes a test tube and a brush or swab. You use that to collect cells from inside the upper part of your vagina (you don’t have to find your cervix). Those cells are sent to a lab, and you get your HPV test results within a few weeks.
There has been a lot of research done on self-collection. Study participants found it easy to collect their own samples. And researchers found that the results matched HPV tests done by providers. The tests are just as accurate.
Preparing for a Pap and/or HPV Test
There are steps you can take to ensure you get the best possible results from your Pap or HPV test.
- Try to schedule the test on a day when you do not expect to be on your menstrual period. If your period begins unexpectedly and will be continuing on the day of your test, try to reschedule the appointment.
- Avoid sexual intercourse 48 hours before the test.
- Do not douche 48 hours before the test.
- Do not use tampons, or vaginal creams, foams, films, or jellies (such as spermicides or medications inserted into the vagina) for 48 hours before the test
Understanding Your Results
There are many different systems that healthcare providers use to classify a Pap test. Within each system, there are different degrees of severity or abnormalities. The various classification systems and degrees of severity include:
Descriptive System: Mild dysplasia, Moderate dysplasia, Severe dysplasia
CIN System CIN stands for cervical intraepithelial neoplasia. Results are classified as CIN 1, CIN 2, CIN 3
Bethesda System:
- ASC-US (Atypical Squamous Cells of Undetermined Significance): Means the results look borderline between “normal” and “abnormal” – often not HPV-related
- ASC-H (Atypical Squamous Cells-can not exclude HSIL):Borderline results, but may really include High-Grade lesions.
- Low-Grade SIL (LSIL) and High-Grade SIL (HSIL): SIL stands for squamous intraepithelial lesion. LSILs are considered mild abnormalities usually caused by an HPV infection. HSILs are considered more severe abnormalities and have a greater chance of progressing to invasive cancer.
Women with abnormal Pap test results are usually examined further for cervical problems. This may involve coming back for a colposcopy and biopsy, or coming back in a few months for another Pap test. If the Pap result is “ASC-US,” then a HPV-DNA test may be done in the lab to see whether HPV is causing this borderline “normal-abnormal” Pap result.
What if Pap test results are abnormal?
If a Pap test shows abnormal cells, additional tests may be performed. These tests include:
- Colposcopy: A colposcopy is an examination of the vagina and cervix using a lighted magnifying instrument called a colposcope.
- Cervical biopsy: In a biopsy, the healthcare provider removes a small amount of tissue for examination under a microscope to look for precancerous cells or cancer cells. Most women have the biopsy in the doctor’s office, and no anesthesia is needed. To do the biopsy, the doctor will insert a speculum to hold the vagina open and take a very small sample. After the sample is taken, it will be sent to a laboratory where another doctor checks the tissue using a microscope. You may experience some bleeding and discharge after the exam and discomfort similar to menstrual cramps. Ibuprofen can be taken to relieve these symptoms.
- Colposcopic biopsy: While viewing your cervix with a colposcope, the healthcare provider removes a tiny portion of abnormal tissue from the surface of the cervix with a special tweezers. The cells are then examined under a microscope.
- Endocervical curettage: A procedure in which the mucous membrane of the cervical canal is scraped using a spoon-shaped instrument called a curette. This can be done in your healthcare provider’s office and does not require anesthesia. There may be some cramping and bleeding after the procedure.
- Cone biopsy: A cone-shaped sample of tissue is removed from the cervix to see if abnormal cells are in the tissue beneath the surface of the cervix. This specimen is much bigger than the biopsy done in the office without anesthesia. A sample of tissue can be removed for a cone biopsy using a LEEP cone procedure, which can be done under local anesthesia, or a knife cone procedure, done in an operating room under local or general anesthesia. You may have some vaginal bleeding for about a week and some spotting for about three weeks after the procedure.
- LEEP (Loop Electro-Surgical Excision Procedure): The LEEP is performed using a small heated wire to remove tissue and precancerous cells from the cervix. This procedure can be done in your provider’s office and requires local anesthesia. There may be some cramping during and after the procedure. You may have moderate to heavy vaginal discharge that lasts for up to three weeks.